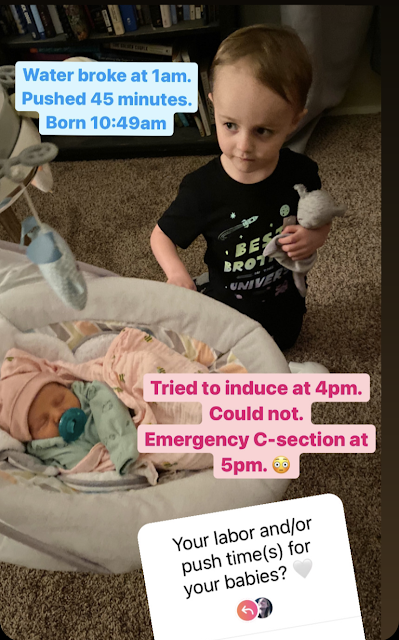
This "push times" sticker had been going around Instagram and I thought, really, that it was just a great way to sum up this baby's birth story:
That's pretty much it. Wells was easy and conventional. Sutton was anything but.
I was checked into the hospital for an induction around noon on March 18th. They wanted to schedule an induction basically because I'm 36 and they diagnosed me with thrombocytopenia. This affected my ability, they said, to have an epidural if my platelet count was low on delivery day (I was skeptical to say the least...this was something I had pre-pregnancy for sure and last pregnancy as well, most likely. I'd never heard anything about it from other doctors.) Plus, I needed penicillin for group B strep. For all of this, they wanted to have me on the schedule for somewhere between 39-40 weeks, instead of letting me go past 40 weeks.
They started the penicillin around 1pm and by 4pm started hooking up the pitocin. So even though we'd been at the hospital since noon, they didn't actually try to induce until around 4:00. I cannot stress enough here that I was nowhere near active labor. I was just there. By the end of this, I never even felt a real contraction.
We also had to go through what felt like a full counseling session with the anesthesiologist during this time and he insisted on a platelet count to see if I'd qualify for an epidural on that particular day. (I never did find out my platelet count but a week after delivery, it was well within normal ranges again, proving that pregnancy had lowered it, which is something that can happen.)
While I was on the penicillin, they noticed right away that the Braxton Hicks were causing some sort of issue with her heart rate. It would drop from 138 to 60 and stay there for minutes. They called it D cells. They had me wear an oxygen mask, change positions, etc to bring it back up to normal. Again, I felt nothing odd or out of place. It was all coming through on the monitors. When her heart rate went back to normal, and they still had no idea what had happened, they started talking about internal monitors. They talked a lot.
The second time her heart rate dropped, they started moving pretty quickly. They broke my water, put an internal monitor on her and, again, I was nowhere near labor. They couldn't deliver her. She wasn't ready. The pitocin had been running for all of like 7 minutes. They decided there was an issue with the cord and the placenta and she was, they surmised, probably squishing the cord with her shoulder when I had a Braxton Hicks contraction.
At this point, they shut off the pitocin and the penicillin and gave me a shot to stop contractions all together.
The next thing I knew, I was in the operating room. There's nothing *quite* as unsettling as a midwife (who doesn't prefer labor interventions) rushing and out of breath as she pushes you down the hallway.
The surgeon came in, introduced herself, and told me what my options were. I don't remember what she said because the fact that I'd already been moved to an operating table kind of told me what my options were.
Since they were able to stop the contracting, they had time to give me a spinal block. Otherwise, it would've been general anesthesia.
I would say it took about 20 minutes for them to set up and deliver the baby. I couldn't see anything, anywhere because of the sheet they had practically over my head. They did let Scott in and told him he could watch whatever he wanted. He didn't take them up entirely on the offer. All I ever saw was the anesthesiologist asking me how I was doing every 30 seconds. I was super lightheaded and tingly and he had to raise my blood pressure at one point.
But...baby Sutton came out yelling. She yelled the entire time they were checking her over and cleaning her up. She was definitely not happy with the turn of events but I was just glad she was out.
Scott and a very nice corporal named Connor, who was the self-described "baby nurse", took her back to the room to wait for me.
I was assured that everything went as well as possible. It was literally a cut-and-dry very easy c-section, despite the rush.
I don't know what kind of drugs they gave me (I know there was morphine) but I spent the next 12 hours throwing up from the narcotics. I do really poorly on any kind of painkiller and this was pretty brutal. I was so thirsty, but if I took more than a sip of water, I threw up. If I tried to raise the bed too vertically, I threw up. Scott completely took care of Sutton for the first 24 hours and then even after that. I *think* I changed maybe one diaper before we got home, but I can't remember.
We went home two days later and I never felt entirely better. Basically, I was just in a lot of pain from the incision and even the meds they sent me with didn't help, but they did make me feel sick so I stopped taking them. I truly don't wish that first week of c-section recovery on anyone. Now, I feel pretty normal 3+ weeks out, but it was not an easy first few days.
The second half of this story is when I did go back for a check-up and had really high blood pressure and they sent me for bloodwork and my labs were a mess and they re-admitted me for three more days and it was a horrible experience and now I hate going to the doctor and have sky-high anxiety and now I'm on blood pressure medication AND anti-anxiety medication and I will probably switch providers because I don't necessarily trust their judgement when it comes to what's actually probably best for the patient.
But I don't want this to be a string of complaints.
I told someone that I should probably be more grateful that they had the skill and the fortuitousness to act swiftly when Sutton was born. She pointed out that maternal medicine still has a long way to go in our country, which is certainly a problem considering that this is America. I agree. Scott thinks we've been stuck in this overabundance of caution cycle because of the way this particular hospital is operating right now. I agree with that too.
All in all, it was not a great experience. However, Sutton is here and she's healthy and I feel on my way back to normalcy.
-------------------------------------------------------------------------------------------
I would be remiss not to add that Scott pulled so much weight in the last couple of weeks. Truly, he thrives during the newborn days in a way that I just do not. Now we're at the point where I've kind of taken over, but he was the manager of Sutton's schedule and swaddling and changing and feeding for the first week at least. I could barely get out of bed in the middle of the night to go check on her so he just slept with her in the living room. This kind of blows me away because I specifically remember not being able to let Wells out of my sight for a long time without panic attacks; with Sutton, she truly did spend most of her first week+ with Scott. I need to say that he was also still working every day, either on his phone from a hospital room, driving in for a few hours, or late at night on his computer. Plus, he remembered to feed the dogs, buy groceries, and cook or buy dinner most nights. My mother-in-law was also invaluable, managing all things Wells for over two weeks, and then taking on a newborn as well when Scott was at work.






Well you weren't kidding when you said it was anything but conventional, geez. Glad you are both ok, and she's here!
ReplyDeleteOH WOW!!!! ... Options? Like, you're on the surgery floor. Did they want you to say, give it some more time - let me push - No surgery for me! ... what a weird thing to talk to you about.
ReplyDeleteUGHHH - that is so miserable to have that nausea for days due to medicine. Thank goodness for Scott!
Blood pressure & anti-anxiety meds - welcome to my world!... Yeah, I'd give it some time for your body to adjust being empty-womb & get rechecked for everything. Your body has gone through the ringer - not a good indication on how things are on a typical day.
I had an emergency c-section with Zoe due to her heart rate plummeting every time I contracted. It was after being in labor for about 24 hours and I was so exhausted at that point. I was in and out of consciousness the entire time, it literally felt like it only took 2 minutes to get her out or something. One minute they were having me spread my arms out, the next they were telling me to open my eyes so I didn't miss seeing my daughter before they took her to clean her up.
ReplyDeleteI am glad that you had Scott and your MIL there to take over baby duty so you could recover. I love how you said they wanted to talk about your options while you were on the table. Umm ok lol. Hopefully your body will even itself back out soon and those meds aren't something you will need to be on permanently.
That was a rough time, and I'm so glad she is healthy and you are getting some help.
ReplyDeleteSo glad things turned out okay in the end. And how great it is that you have a strong support system.
ReplyDeleteKristin. I don’t even have words. I’m so thankful you both are on the other side.
ReplyDelete